Establishing the process
In the recruitment process, establishing the procedure, criteria and timings before a call for applications sets up a rigorous and fair selection process. It can become difficult to have discussions around decision-making processes at peak times during the recruitment process, particularly when the focus shifts to establishing interview panels and Selection Committee members’ fielding multiple requests of their time.
Have a kick-off meeting
Start the process by gathering the whole Selection Committee, along with your HR department. It may be hard to include all members, but a core group should initiate the process.
Despite policy possibly instructing Selection Committee to form only when candidates are under consideration, involving committee members in the position description design or redesign is valuable. Their input and experience can assist in developing and streamlining the candidate selection process and increase the likelihood of consensus among committee members about the process and selection of candidates.
Review key documents
In the planning stage, it is useful to review any data and information from previous years of recruitment alongside any jurisdictional or RACP policy changes. This information can prompt a need to consider changing the position description or the selection process.
Key RACP documents:
Equity and diversity
The idea of 'workplace diversity' means that a workplace should reflect the makeup of our broader society. This is acknowledged as a key issue by the Australian and New Zealand Governments and the RACP.
One of the four RACP principles for selection is embracing diversity to engage a more diverse range of candidates to apply for and progress through training. It is also a key priority of the RACP Indigenous Strategic Framework to support the increased selection of Aboriginal and Torres Strait Islander and Māori physician trainees, in partnership with training providers, to grow the Indigenous medical workforce.
Training providers should demonstrate a strong commitment to equitable selection and health outcomes for Indigenous peoples in Australia and Aotearoa/New Zealand4 as well as people living in regional, rural or remote regions, and other under-represented groups.
An inclusive workplace culture is one where all staff are valued and recognised for their unique qualities, ideas and perspectives. Acknowledgment of the skills and perspectives that staff may bring to the workplace through their race, gender, culture, disability, age, sexual orientation, gender identity or other differences, can contribute to a better workplace and organisational outcomes5.
Although there is no set approach to what factors should be considered in relation to addressing equity and diversity in selection outcomes, the first step is to make equity and diversity obligatory discussion for the selection committee. The committee should research how well the program is currently performing in ensuring diversity in its trainee workforce.
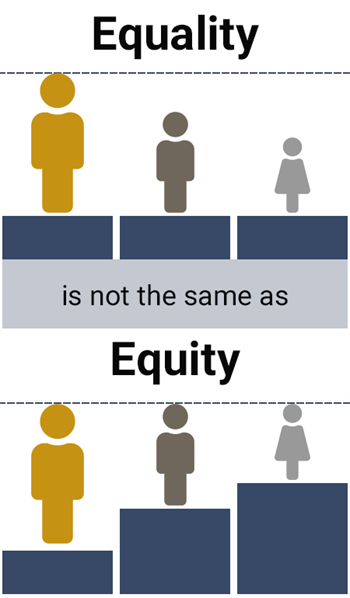
Members may feel that if the selection process itself is fair and open to all, and that there are no obvious signs of discrimination, then this should be sufficient evidence of a ‘level playing field’. However, it is important to challenge ideas like this that assumes all candidates arrive from the same starting point. Some trainees may have had more barriers to overcome than others in entering medical school and progressing through to applying for Basic Training or Advanced Training.
Have a conversation around the differences between the concepts of equality and equity. After your discussion, review the process of selection and recruitment to consider whether more equitable selection outcomes can be achieved through any changes or additions.
Resources and timelines
Discuss and allocate responsibility for all part of the process and what level of administrative support will be required. Create and share a timeline flagging key dates and have instruct all committee members to block out the proposed interview period to avoid conflicts.
The training needs of Selection Committee members and support staff should be reviewed by the Chair early in the process.
Plan the process
Recruitment and selection should be conducted in accordance with RACP Training Provider Accreditation Standards, particularly the principles of fairness, rigour and transparency, and within legal requirements including anti-discrimination legislation.
Following a proper process and abiding by legal obligations is in everybody's best interest.
Under New Zealand and Australian laws, employers are required to provide equal employment opportunities and make hiring decisions based on individual merit. It is unlawful to treat a candidate less favourably because race, sex, sexual orientation, age, disability, marital or domestic status, family or carer responsibilities, pregnancy (including breastfeeding), religion, political opinion or criminal record.
There may be some limited exceptions where these characteristics are genuinely relevant to the candidate's ability to perform the role, but generally it is unlawful to treat a candidate less favourably because of these attributes.
To minimise the risk of discrimination in recruitment, consider the following criteria:
- Are you planning your approach to comply with your obligations to prevent discrimination?
- Are you being consistent and fair in the way you treat applicants?
- Are you sure no irrelevant personal information from applicants has been sought?
- Are you focusing on the essential requirements of the role?
- Are you setting aside personal bias, myths and stereotypes?
- Are you considering what can be done to accommodate applicants who require adjustments?
Consultation
Your local HR department or workforce unit should be consulted throughout the entire selection process. They are particularly vital in addressing any queries about the process, requirements, employment policies, training, providing support and guidance and assisting with significant process changes and resourcing issues.
If you are recruiting for positions within a network of settings, there will likely be a key person appointed to coordinate this activity. Generally, this person will coordinate a meeting between sites. If recruitment is not being coordinated centrally, then it is important to liaise with this key contact to ensure all proper processes are being followed. An agreed framework for position descriptions and selection may already be established.
Candidates assessment
For reasons of rigour and fairness, it is important to agree ahead of time how you will be deciding on candidates. Many factors go into obtaining the best recruitment outcomes, including:
- how many assessment tools are used
- the use of specific assessment tools
- the breadth and training of Selection Committee members
- how and when candidates are scored, such as what weighting or scoring rubrics is used and when
Recruitment process snapshot
- Engage selection committee and confirm support resources
- Identify and confirm the numbers of positions to be recruited
- Perform position analysis (if required) and design
- Set dates for information sessions and interview panels
- Application review and culling meeting
- Closing date for application
- Finalise website information
- Final date for confirming positions and upload to recruitment system
- Interviews
- Reference collecting
- Selection committee report due
- Job offer and contracting phase