There is a full range of team members (medical, nursing, allied health and other staff) with an appropriate skill base and training to provide comprehensive, contemporary programs of care to address the impairments, activity limitations and participation restrictions present in the patients admitted to the rehabilitation medicine service. There are sufficient team member hours available to allow each patient to receive an individualised nursing and allied health program of adequate intensity7, 8, 9, 10 to meet their needs, delivered in a way that optimises the effectiveness and efficiency of the rehabilitation program.
Demonstrating the standard
2.1 Staffing of the Rehabilitation Medicine Service
2.1.1 The staff establishment for a rehabilitation medicine service includes an adequate number of professional and support staff to allow the service to provide contemporary, evidence-based rehabilitation management in a safe, effective and efficient manner.
Staffing levels need to be reviewed regularly and particularly when new models of care, such as acute rehabilitation or in-reach rehabilitation, are introduced.
Medical staff
2.1.2 Each 10 inpatient beds within the rehabilitation medicine service should have either 0.5 FTE rehabilitation medicine physicians (Amputation, Orthopaedic, Major Trauma, Pain, Reconditioning / Restorative and other impairment groups) or 0.8 rehabilitation medicine physicians (Stroke, Neurology, Traumatic Brain Injury (TBI), Spinal Cord Dysfunction). These staffing levels are inclusive of the requirement for pre-admission assessment of patients and for routine follow-up of patients of the service.
2.1.3 Ideally inpatient services will have allocated junior medical staff (Rehabilitation Medicine trainees and other Resident Medical Officers (RMO). Specific staffing numbers for junior medical staff will vary depending upon the casemix of the inpatient rehabilitation medicine service and the acuity of patients e.g., where the inpatient service manages patients of higher acuity, such as patients with recent spinal cord injury or acute stroke, junior medical officer numbers will need to be higher than the minimum numbers outlined at 2.1.5 (below). N.B. In this document the term RMO is used to describe all junior medical staff who are not Rehabilitation Medicine trainees.
2.1.4 As a guide, it would be expected that for every 10 inpatient beds there would be a minimum 0.5 RMO and 0.5 Rehabilitation Medicine trainees. These minimum numbers apply only to the provision of direct inpatient care (for example, attending to the individual medical needs of patients, ward rounds, case and family conferences, and some pre-admission assessments and follow-up). Where trainees undertake additional duties (for example, active involvement in community rehabilitation services, outpatient programs and assessing patients in acute care) then additional trainee hours are required to support the inpatient rehabilitation beds.
2.1.5 In some situations, a Career Medical Officer (CMO) or in NZ a Medical Officer of Specialist Scale (MOSS) may replace a RMO or trainee.
2.1.6 In the occasional situation where there is no RMO / CMO / MOSS, Rehabilitation Medicine trainees should be responsible for the day to day management of a maximum of 20 inpatients.
2.1.7 In some situations, the junior medical staff duties may be covered by an additional allocation of rehabilitation medicine physician time.
2.1.8 Each rehabilitation medicine service which has Rehabilitation Medicine trainees must obtain accreditation11 with AFRM as suitable for advanced training in rehabilitation medicine.
2.1.9 There is sufficient medical staffing to provide a suitable after-hours medical roster.
Nursing staff
2.1.10 The nursing team must be led by a full-time nurse with relevant training, expertise and qualification in rehabilitation. This nurse will be the manager of the unit (supernumerary to direct care provision) and will lead the nursing and operational aspects of the unit.
2.1.11 Nursing staff numbers are to be sufficient to ensure the safe and effective nursing management of patients within the service. The majority of nursing staff will hold qualifications/experience in rehabilitation. Each service must demonstrate its professional nursing specialisation compliance with the appropriate nursing standard or framework.
Note: For further details about nursing standards and competencies please refer to the Australasian Rehabilitation Nurses’ Association (ARNA).
2.1.12 Nursing staff within a rehabilitation medicine service also have responsibility for participation in the rehabilitation needs of patients to facilitate patient recovery and independence. There shall be sufficient nursing care hours (over a 24-hour period) for nursing staff to deliver, facilitate and reinforce therapy programs. This is especially important after business hours and on weekends and public holidays.
2.1.13 Nursing staffing hours should be sufficient to ensure full participation in all interdisciplinary team processes including case conferences, team meetings, goal planning meetings and family meetings as well as in patient and staff education and teaching activities.
2.1.14 All nursing care, over the entire 24-hour period, must be under the supervision of a registered nurse.
2.1.15 The service shall employ nursing experts according to the rehabilitation casemix (such as Continence, Wound, Pain, Stomal nurses). The nursing service must have an active practice development plan which clearly reflects the education and learning needs of rehabilitation nurses.
2.1.16 There should be a preponderance of registered nurses over enrolled nurses and assistants in nursing.
2.1.17 Nursing hours may need to increase if the rehabilitation medicine service caters for patients with acute medical issues and /or high nursing dependency.
2.1.18 It is recognised that individual rehabilitation medicine services may have their own methodology for determining nursing numbers (for example, load ratios). However, where that is not the case the following can be used as a guide to nursing staffing levels for a rehabilitation medicine service: For each 10 inpatient beds, there should be a minimum of 11.75 FTE nursing staff. This number may rise to 14.75 FTE for services which require greater nursing intensity, such as spinal cord injury rehabilitation. These figures include the Nurse Unit Manager, but do not include the Clinical Nurse Consultant or the Nurse Educator which are recommended at ratio of 0.5 FTE for each 10 inpatient beds.
Allied Health and Other Professional Staff
Table 1: Allied Health Staff to Patient Ratios for each 10 Inpatients
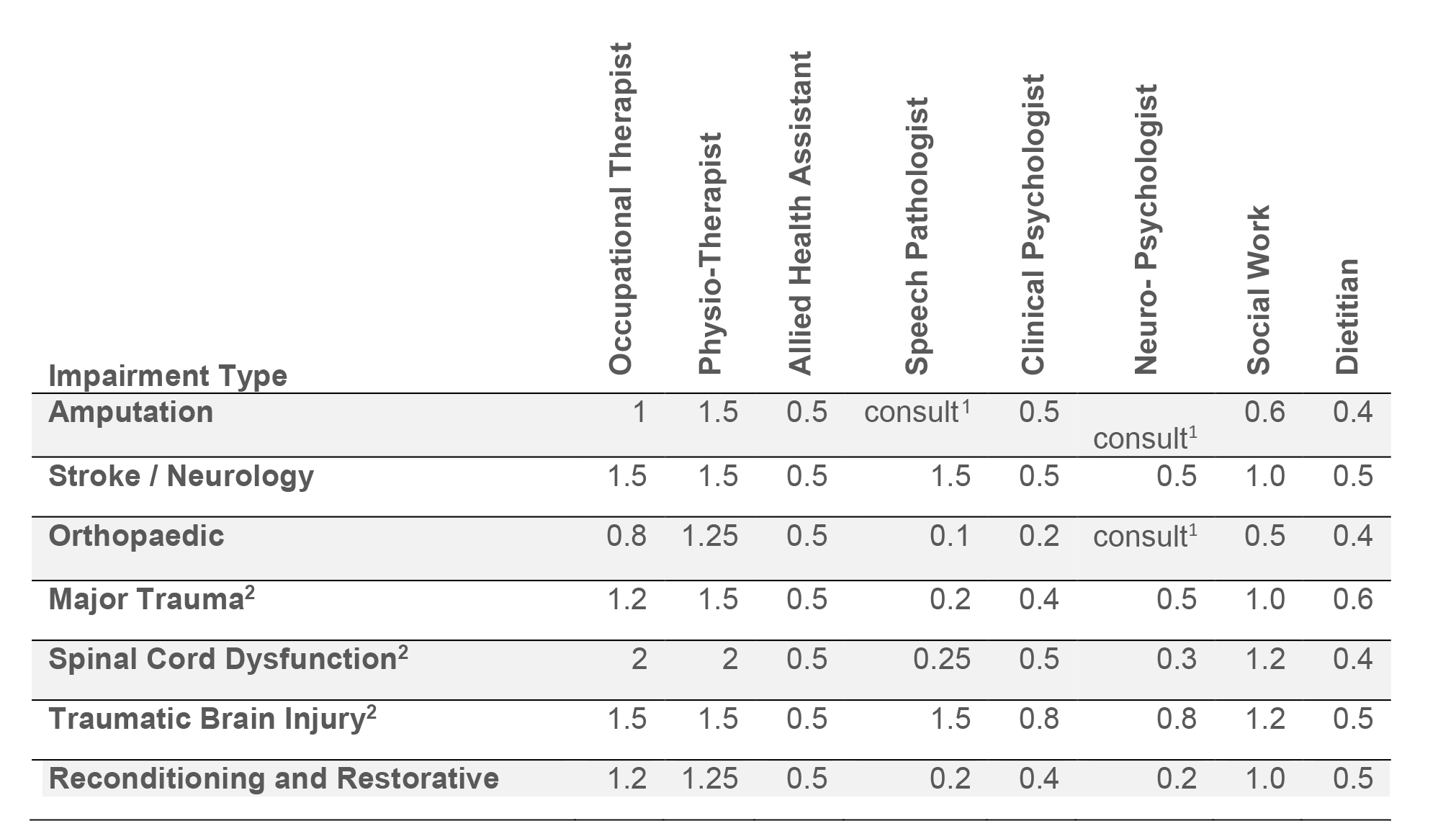
1 ‘consult’ denotes the availability of staff on a consultation basis, as required.
2 Major Trauma is defined as complex injuries to multiple body systems that may also include spinal cord dysfunction and/or traumatic brain injury (TBI).
Notes:
a. This table provides indicative of staffing levels for a five day per week rehabilitation program. A six or seven day per week program requires additional staffing. Refer to 2.1.26.
b. The staffing levels outlined in this document do not include staffing sufficient to relieve staff who are on leave.
c. The staffing levels do not include time required for teaching and research activities.
e. Prosthetist / Orthotist: See section 2.1.33 and 2.1.34.
2.1.19 Patients admitted to the rehabilitation medicine service will receive an appropriate quantum and mix of therapy to enable them to achieve an optimal rehabilitation outcome within an appropriate timeframe. This will vary according to individual patient factors such as the nature of the patient’s impairment, the time since onset of impairment, the presence of co-morbid conditions, the patient’s ability to tolerate therapy, their cognition and their motivation to undertake rehabilitation. There is mounting evidence in the literature on the benefits of greater therapy intensity in improving functional outcomes and improving the efficiency of the rehabilitation process7, 8, 9, 10.
2.1.20 The ultimate determinant of the staffing levels will be the type and intensity of therapy needed by patients in the unit, to meet their requirements. While the staffing ratios outlined in Table 1 are a useful guide to the overall allied health staff establishment required, the aim must be the delivery of appropriate rehabilitative therapy12.
2.1.21 The appropriate amount of therapy that patients receive will be a minimum of three hours per day for patients who have the capacity to tolerate this amount of therapy. This should occur on a minimum of five days per week.
2.1.22 ‘Therapy’, as used in 2.1.19, generally includes physiotherapy, occupational therapy, and speech and language therapy, delivered by professionally qualified and skilled staff, or by allied health assistants under the supervision of professionally qualified allied health staff. Therapy can be delivered on either an individual or group basis, but if delivered on a group basis the patient must be an active group participant and must be following an individually tailored program. Therapy can also include that delivered by other professional disciplines, such as defined in 2.1.36 or other professionally qualified staff, depending upon patient need.
2.1.23 Table 1 provides guidelines for allied health and allied health assistant staffing of the rehabilitation medicine service at the unit level. However, there may be a high degree of variability between the casemix of different rehabilitation medicine services and this must be considered in determining the allied health levels for different services.
2.1.24 As well as adjusting staffing levels to suit the casemix of the rehabilitation medicine service, the staffing levels for allied health and allied health assistants must also be adjusted to account for the percentage of time that these staff have available for the delivery of direct patient care. In essence, only a percentage of the time that a therapist has available to them is ‘patient attributable’ time. Only a percentage of ‘patient attributable’ time is available for direct patient care, because ‘patient attributable’ time also includes other patient-related activities such as attending case and family conferences and ward rounds, writing reports and travel.
2.1.25 In cases where allied health staff are to be available on a consultation basis, the consultation should occur in a timely manner so as to not interfere with the rehabilitation program or prolong the inpatient rehabilitation episode.
2.1.26 Staffing numbers might need to be adjusted if the Rehabilitation Medicine service caters for patients with special needs (for example, bariatric patients, or patients with infection control requirements), as the time taken for staff to deliver effective therapy programs in these circumstances is greater. Specialist rehabilitation medicine services are likely to require a higher level of allied health staffing including those that manage a complex caseload e.g. people with dual diagnoses, challenging behaviour, substance misuse and dementia.
2.1.27 The provision of therapy on weekends is strongly recommended as it has been shown to increase functional independence, physical activity, quality of life and in some cases, reduce length of stay13, 14.
2.1.28 There should be sufficient staff to meet the psychosocial needs of patients.
2.1.29 There should be sufficient staff to allow relevant rehabilitation team members to participate in case and family conferences and ward rounds, when required.
2.1.30 The services of a neuropsychologist are essential in services where patients with brain impairment are managed.
2.1.31 Clinical psychologists are employed in all units where patients with complex behavioural issues are treated and where adjustment to the disability may be an issue.
2.1.32 Brain impairment and spinal cord dysfunction programs have access to an outreach team comprising appropriate medical, nursing and allied health staff.
2.1.33 Amputee rehabilitation programs have close liaison with prosthetists who are able to provide a comprehensive prosthetic service and who attend assessments when prostheses are prescribed.
2.1.34 Close liaison with an orthotist is required for stroke and neurological patients, major trauma patients, and those with spinal cord dysfunction and traumatic brain injury. If prosthetists / orthotists are not part of the employed staff establishment, then arrangements with a private provider are to be made.
2.1.35 The majority of patients in a rehabilitation medicine service will require input from pharmacists. The pharmacist should be an integral part of the rehabilitation team.
2.1.36 Nominated staff from other disciplines such as exercise physiology, podiatry, diversional therapy, music therapy, leisure therapist / recreation officer or therapist, rehabilitation counselling, sexual therapy, rehabilitation engineering and vocational rehabilitation should be available as required.
2.1.37 Access to health care interpreters must be available to allow optimal comprehension of rehabilitation, goals and overall process.
2.1.38 Cultural support services, culturally appropriate goals and acknowledgement of cultural norms for certain patients where appropriate, should be in place.
Support Staff
2.1.39 Each rehabilitation medicine service should have available adequate numbers of support staff to ensure the effective running of the service.
2.1.40 Administrative support is required to ensure that rehabilitation outcomes data are collected and entered onto an appropriate database and submitted to the relevant health authority and to AROC.
2.1.41 Staff to assist in the movement of patients to therapy areas should be available if required so that therapy programs can be scheduled without interruption and without using treatment time of allied health and nursing personnel.
2.1.42 There should be adequate cleaning staff to meet the needs of the service and to cater for patients with infection control issues.
Other comments regarding staffing
2.1.43 Nursing staff levels should be adequate to ensure that the rehabilitation medicine service is able to provide appropriate rehabilitation support outside of usual business hours, to allow patients to progress with their rehabilitation program during these times.
2.1.44 The use of family and appropriately trained volunteers in rehabilitation programs should be encouraged and supported.
2.1.45 The use of formal peer support services or involvement of people with similar disability should be encouraged in rehabilitation services when appropriate.
2.1.46 Staffing levels for the rehabilitation medicine service must reflect the needs of the service to safely manage acute medical and surgical issues as they arise without disrupting the care of other patients.
2.2 Human resource management
2.2.1 The service is directed by a rehabilitation medicine physician.
2.2.2 The Director of the Rehabilitation Medicine Service (rehabilitation medicine physician) is responsible for the co-ordination of treatment and the monitoring of standards of treatment.
2.2.3 Each inpatient rehabilitation service will have appointed a Nurse Unit Manager. The Nurse Unit Manager will be responsible for professional services and operational requirements of the service related to nursing.
2.2.4 There is documented evidence of a line of responsibility from the person in charge of the service to a senior administrator.
2.2.5 The senior clinician of each discipline is responsible to the Director of the Rehabilitation Medicine Service for the standard of clinical service provided by all practitioners in that discipline.
2.2.6 Each allied health professional staff member is responsible for the quality of care given to individual patients under the overall care of the assigned rehabilitation medicine physician.
2.2.7 In each clinical unit there is at least one senior therapist assigned permanently. Junior staff in the same discipline may be rotated to facilitate their professional development. However, if this occurs, due consideration must be given to the impact on clinical services in that discipline and on the service as a whole.
2.2.8 The nursing staff is sufficient in number and have appropriate experience to fully perform the nursing duties necessary for the proper care of patients and safety of staff at all times. Nursing requirements vary according to the nature of the disability and reflect the recorded dependency scale of the patients.
2.2.9 All staff are adequately skilled, qualified and knowledgeable about rehabilitation in order to perform their duties professionally and effectively.
2.2.10 The rehabilitation medicine service and the relevant hospital administration recognise the need for staff to maintain and develop their skills and knowledge. In order to provide staff capacity to do so there must be provisions within industrial awards as well as through funding support for continuing professional development.
2.2.11 Within the organisation there is a current list of all professional staff including their qualifications, experience and duties. This list is updated annually and includes evidence of registration with the appropriate Board or agency with evidence that qualifications have been verified and compliance with continuing professional development requirements are confirmed.
2.2.12 There is a position description for each category of professional position.
2.2.13 Specialised procedures are undertaken only by staff with appropriate qualifications and experience. An appropriate credentialing process and quality monitoring is established.
2.2.14 Where the service’s staffing complement does not contain a full range of the professional expertise required, there are documented arrangements for referral to outsourced professionals to provide the required expertise.
2.2.15 Annual staff appraisal is conducted with appropriate documentation. These are performed by each staff member’s discipline specific supervisor and overseen by the Director.
2.2.16 There is a documented management review process, which regularly reviews and adjusts the overall staffing needs of the organisation.