Aboriginal people comprise about 45% of the Kimberley region’s approximately 36,000 strong population.
Among this group, cardiovascular disease (CVD), diabetes and rheumatic heart disease (RHD) are reported at higher rates than in the non-Indigenous population, as are comorbidities and complex health and wellbeing challenges. But almost half the Aboriginal population are under 20 years of age. A longer term goal is to increase the health of the future adult Aboriginal population by focusing on the health of expectant mothers, the unborn, infants and children. Specialist services are critical in this context.
Snapshot | Kimberley
 The 30 or so language groups of the Garadjeri, Bardi and Ungarinyin Aboriginal Nations have occupied the Kimberley region of northern Western Australia (WA) for tens of thousands of years.
The 30 or so language groups of the Garadjeri, Bardi and Ungarinyin Aboriginal Nations have occupied the Kimberley region of northern Western Australia (WA) for tens of thousands of years.
Today, hundreds of Aboriginal communities of various sizes are scattered throughout the 425,000 square kilometre sized area (twice the size of Victoria). Broome, the major centre (population of about 14,500 in 2016) is over 2000km by road from Perth and was founded in 1883 to support the pearling industry.
Other towns are Derby (3300), Fitzroy Crossing (1200), Halls Creek (1500) and Wyndham (800). A thousand kilometres north-east of Broome, Kununurra (5500) was founded in 1961 as the Ord River Irrigation Project’s service town.
Case study | Kimberley specialist services
The Western Australian Primary Health Alliance operates the State’s three Primary Health Networks (PHN). Country WA is the local PHN and the Aboriginal Community Controlled Health Services (ACCHS) are a critical part of the primary health system across the region.
Established in 1986, Kimberley Aboriginal Medical Services (KAMS) supports and represents the interests of a regional environmental health service and six independent ACCHSs based in Beagle Bay, Broome, Derby, Kununurra, Halls Creek, Balgo, Billiluna, Mula and Bidyadanga, the largest discrete, remote WA Indigenous community with about 750 residents.
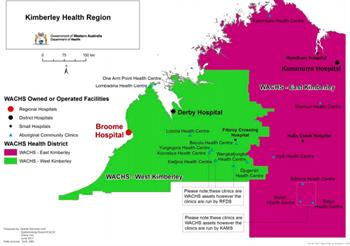
At the secondary and tertiary level, the WA Country Health Service’s (WACHS) major hospital is at Broome, with smaller hospitals at Derby, Kununurra, Halls Creek, Fitzroy Crossing and Wyndham — as illustrated in the map.
The Kimberley Regional Physician Team includes three WACHS-employed general medical consultants (one dual trained in respiratory medicine) and two registrars. The latter are primarily funded through the Specialist Training Placement and Support scheme with support from WA Health. The team work in rotation across the region with half of its members at any one time in Broome, and the other half working across 22 other sites including the smaller hospitals, ACCHSs clinics, regional prison and other remote health services. If necessary, patients are transferred to metropolitan Perth hospitals or, less commonly, the Royal Darwin Hospital for treatment.
Cardiovascular disease, including rheumatic heart disease, is a major cause of morbidity and mortality for Aboriginal people across Australia, including in the Kimberley. Private Perth-based Perth Cardiovascular Institute (PCI) were contracted by WACHS in 2018 to provide cardiac specialist services to Kimberley public patients. PCI cardiologists visit clinics, including in ACCHSs, across the region each month and support access to angiography, coronary artery bypass grafting, valve replacements and so on including at metropolitan hospitals in Perth.
In addition to supporting management of cardiac morbidity within the region, it is anticipated that PCI’s establishment of relationships with community members over time will also assist with continuity of care for people undergoing treatment in Perth. Royal Perth Hospital Nephrology provide visiting clinics at multiple sites within the region and support the provision of satellite haemodialysis across the region through Kimberley Renal Services.
The other visiting medical specialty is rheumatology, with two visits provided per year from Perth-based consultants to support the health of mothers, infants and the future adult population of the region, obstetric and paediatric teams based in Broome provide clinics across the Kimberley.

The region’s ACCHSs and the Kimberley Regional Physician Team have a long-standing relationship. In addition to team members providing clinics at ACCHSs, this also includes them running teaching sessions for GPs and GP registrars and an annual regional Chronic Disease Workshop.
Culturally safe working practices are critical to the success of the Kimberley Regional Physician Team’s work with Aboriginal patients particularly in hospitals, and cultural competence in treatment is important regardless of setting. Team cultural awareness training and working with local Aboriginal Health Workers and Aboriginal Liaison Officers in hospitals and local clinics is critical to ensuring this.
Provision of physician clinics across the health services in the region is based on projected demand based on what population data is available, and modified based on referral numbers. Logistical arrangements to ensure coverage across the region’s 20+ health sites requires the complex coordination of road, light plane travel and accommodation. A particular challenge is to manage the distances required in an efficient way, particularly as the demand on health services already outstrips staff capacity.
Attracting long-term staff to the region is key to improving regional population health. The continuity of care made possible by long-term regionally based staff not only makes for a better patient experience and outcomes, but also supports the efficiency of the regional health system. Dr Lydia Scott, who has worked within the Kimberley
Regional Physician Team since 2015, describes the rewards and challenges involved.
 “There is a huge appeal to working as general physicians in areas like the Kimberley, with experiences possible that would not be available elsewhere and that keep things interesting. I work in a range of ever-changing scenarios, with inpatient and outpatients, in clinics, and Indigenous remote communities.
“There is a huge appeal to working as general physicians in areas like the Kimberley, with experiences possible that would not be available elsewhere and that keep things interesting. I work in a range of ever-changing scenarios, with inpatient and outpatients, in clinics, and Indigenous remote communities.
"Teamwork is essential here, and you are always working with professionals and people from other disciplines who are passionate about good healthcare, and Aboriginal health in particular. Working remotely and in relatively small towns, you quickly become part of the community.”
— Dr Lydia Scott on working in the Kimberley