Professor John Wilson welcomed attendees and acknowledged that Directors of Physician Education (DPEs) are an important part of making and implementing College education policies.
The purpose of this forum was to:
- provide an update on the RACP Education Renewal projects including:
- Basic Training curricula renewal
- Advanced Training curricula renewal
- other related Education Renewal projects
- understand the role and objectives of the Adult Internal Medicine Basic Training Committee
- explore the needs of DPEs and the need for such national forums ongoing
Education renewal and AMC accreditation
Robyn Burley, Director of Education, Learning and Assessment provided forum participants with an update on the current status, plans and timelines for the RACP Education Renewal projects, including:
- Curricula Renewal: Basic and Advanced Training
- examinations
- Accreditation Renewal
- supervisor training
- physician health and wellbeing
- AMC accreditation
The RACP Education Renewal Program is designed to enhance the quality education services that the RACP delivers, to transform the business processes that support these services and ultimately to better serve the health of patients, carers, communities and populations. The program comprises a series of significant interrelated projects that will be delivered over the coming years.
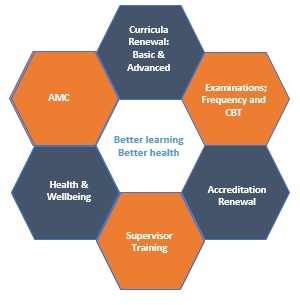
Figure 1: RACP Education Renewal Program
SPDP workshops
The participants sought clarity on the availability of the SPDP and SPDP facilitator training workshops.
AMC and MCNZ accreditation
The College successfully supported a mini-visit by the AMC/MNCZ in late 2018.
The journey so far – the history of PREP
A/Professor Mitra Guha gave an overview of the journey of the Basic Training programs and the roll out of the Physician Readiness for Expert Practice (PREP) programs.
The forum participants discussed the need for more robust processes for trainees in difficulty to be developed, with increased provision for DPEs supporting these trainees
It was agreed that the College has a role in supporting DPEs and ensuring their wellbeing in the discharge of their responsibilities
Basic Training Committee – roles and objectives
Dr Ann Gillett, Chair, Adult Internal Medicine (AIM) Basic Training Committee, provided an overview of the:
- role and objectives of the AIM Basic Training Committee in Basic Training
- roles and responsibilities of Committee members
The Adult Internal Medicine Division Basic Training Committee was established to ensure oversight in the implementation of College Education Policy in the Adult Medicine Division Basic Training program nationally, including minimum PREP requirements, accreditation, examinations and supervision, working collaboratively with DPEs and relevant New Zealand committees.
The participants heard from their state DPE representatives on the Committee about:
- roles and responsibilities of Committee members in managing the training program requirements and handbooks, discussing trainee applications for special consideration and other issues brought up by trainees and DPEs
- NSW DPE representative spoke of the benefits of BPT training networks within NSW, which allows for:
- distribution of trainees (across metropolitan and regional sites)
- integration of rural sites into network to ensure all training program requirements are met
- a greater breadth of experience for trainees, with exposure to various settings and rotations
- Adult Medicine Chair of the Written Exam Committee spoke of the work being undertaken to increase the question bank and the processes of writing exam questions and setting the Written Examination. Participants were encouraged to sign up with the Assessment Unit to become question writers.
The participants raised/discussed the following matters:
- benefits of the creation of local selection processes and/or selection panels for recruitment and entry into Basic Training
- benefits of, and a greater need for, DPE mentorship
- future shape of assessments – the experiential growth of medical knowledge and the challenges faced
- need to change the way the College communicates with DPE and trainees
College Learning Series
A/Professor Mitra Guha, provided an overview of the College Learning Series (CLS).
The College launched the College Learning Series on 12 February 2018. This is a comprehensive online learning resource designed to support Basic Trainees with a schedule of recorded lectures mapped to the new Basic Training curricula standards.
There has been great uptake of the lecture series by Basic Trainees, Advanced Trainees, Fellows and overseas trained physicians.
Clinical Examination Committee/CLEAR
Dr Elizabeth Whiting, Chair, Divisional Assessment Committee, spoke to the:
- purpose of the Clinical Examination
- importance of redefining the marking rubric to match domains
The purpose of the Clinical Examination is to assess the trainee’s clinical skills, clinical acumen and interpersonal skills to determine whether they have reached the standard for completion of Basic Physician Training.
The participants discussed:
- importance of redefining the marking rubric to match domains
- achieving the right balance between long and short cases and ensuring they complement each other; but have emphasis on different aspects of a clinical assessment
- there is no longer a 'pass mark' - trainees should be seeking to do well in both the short and long cases
Accreditation
A/Professor Alistair Reid, Deputy Chair, Accreditation Subcommittee, presented and participants discussed the:
- importance of accreditation in helping hospital improve settings and training environments
- accreditation being viewed as a resource for DPEs to advocate for training excellence
- future state for accreditation and the training provider standards and training program requirements
- uptake of counselling services accessed by trainees and supervisors has increased (identified as part of the Physician Training Survey)
The objective of the College’s accreditation renewal project is to design and implement a coordinated accreditation program that assesses rotations, training programs, settings and networks against a new set of accreditation standards with comprehensive processes.
Support for trainees and supervisors
Dr Spencer Toombes, Deputy Chair, AIM Basic Training Committee, held a brief interactive workshop where participants discussed:
- importance of identifying what can cause trainee stress and how that impacts on their work and home life
- identifying areas where trainee stress could be reduced on an individual, supervisor (DPE) and employer basis
- importance of understanding the role of the hospital – service vs training
- importance of understanding and defining the role of DPEs – are you a supervisor, mentor or assessor
- recognising that trainees are pulled in a number of different directions – it's about finding balance between those directions and building symbiotic relationships
- stress vs resilience – recognising that this is a difficult job and it's important to help trainees manage stress, rather than distress
- building a community of support for trainees and encouraging community in hospitals
The Adult Medicine Council acknowledges that training requirements, rotation accreditation and examination processes contribute significantly to trainee stress. The Council have proposed that the College review and adjust these processes to improve transparency and fairness with the aim of reducing their potential negative impact on trainee mental health and wellbeing.
DPE development
Dr Malcolm Turner, VIC/TAS state DPE Group Chair, presented and participants discussed:
- understanding and identifying the different areas for development as a DPE
- importance of creating a close local and broader network of support (including mentorship). This includes the creation of an online platform for community of practice to share knowledge and experience
- predictable (and unpredictable) aspects of the role – making sure that DPEs understand what is required of the role and how they can be supported by their peers.
- structural components of Paediatrics & Child Health DPEs and understanding how they maintain a reduced turn-over compared to Adult Internal Medicine DPEs - an audit of the current and future data to determine how many DPEs there are, how long they stay in this role and why they leave, was suggested
- importance of having a clear structure and guide for trainees in difficulty (including exiting trainees from the training program) - several concerns were raised about how and where DPEs could seek support in such situations, rather than making a substantive decision on their own
FAQs and open discussion
The participants discussed:
- capacity to train, including:
- need to ensure quality training and adequate rotation exposure
- capacity for the Clinical Examination and how this will affect the number of available training positions
- selection into training process and how the creation of a single-entry point into training, coupled with a recruitment/ranking process to assist DPEs
- acknowledging that workplace practices are changing, which means there is an increase of junior doctors joining the workforce
- managing the expectation of potential trainees
- advocating for the availability of flexible training options (e.g. job share opportunities) within the workplace
- exit points for training, including:
- providing a qualification or completion certificate for trainees who have been successful in completing Basic Training, but do not move onto Advanced Training
- professional recognition for trainees who decide to pursue a career as medical registrars/hospitalist
- alternative pathways, including obtaining qualifications through a specialist society (although not accredited/recognised by the AMC)
- trainees in difficulty, including:
- identifying and communicating marginal trainees between supervisors and hospitals to ensure adequate support is provided
- ensuring a clause/condition of employment is provided that ensures trainees are aware that information will be transferred between sites and supervisors regarding progression through training
- placing the responsibility of reporting previous issues on the trainee may not be the most effective method
The Forum concluded at 4pm with agreement that the dates of the next forum would be communicated as soon as possible and DPEs would be surveyed to determine topics for discussion.
Participants, presenters and RACP staff were thanked for making this a successful forum.