Priority 4: Foster a culturally safe and competent College
Competence in Indigenous health matters is not the same as Indigenous cultural competence. In Aotearoa/New Zealand cultural competence is recognised as a key professional skill required to address health disparities for Māori, as enshrined in legislation through the Health Practitioner’s Competence Assurance Act 2003. Both the MHC and ATSIHC consider that clinical competence is not possible without cultural competence; and it provides the foundation for equity and collaboration. Both committees are guardians of cultural competence in the RACP. They articulate the values of cultural competence, and mediate their translation into RACP systems and processes.
Cultural competence is a central skillset and a key area for the College to work consistently to achieve the principles of the Te Tiriti o Waitangi (the Treaty of Waitangi). Cultural competence is also a core component of the RACP’s accreditation processes and assessed by the regulators, the Australian Medical Council (AMC) and the Medical Council of New Zealand (MCNZ).
Being culturally safe means that we recognise and ameliorate the impact that our own beliefs, assumptions, and behaviours have on others; and, for health care practitioners, recognising the serious adverse impacts on patients and whānau (family) of practicing in a culturally unsafe way. The impacts can be long‑term and widespread, reaching far beyond any one specific incident.
Within the RACP, cultural competence is implicit in all aspects of physician and paediatrician education, training, professional development, and practice. Cultural competence requires awareness of cultural diversity, understanding of issues faced by different populations, and the skills to function effectively and respectfully when working with people of different cultural backgrounds.
It is in these key areas that Indigenous cultural competence is differentiated from broader definitions of this concept. It is within the power of the College to lead the way in delivering culturally competent health care to Aboriginal and Torres Strait Islander peoples, Maori, and Pacific peoples.
The RACP must train doctors to be culturally competent so they have the skills, knowledge, understanding, and practices to work in a safe and effective way with patients and whānau (family), to improve health equity and health outcomes. Culturally competent doctors understand that:
- Populations are culturally diverse
- The doctor’s own culture and belief systems influence their interactions with patients and whānau (family), who may have a different perspective
- Positive outcomes are achieved when people’s experiences are acknowledged and when doctors treat patients and whānau (family) with respect.
The RACP has a key responsibility to provide access to role models, mentors, and teachers that can help equip doctors meet the needs of populations, and it is important that the RACP systematically record the ethnicity of its members through targeted resources and support. There are many examples whereby the cultures of health care and hospital systems have worked as a barrier to cultural competency. The RACP can change health and hospital culture for the better. The RACP can use its Curriculum Framework to set standards for culturally diverse praxis, in constructive critique of Western biomedical and biopsychosocial models. The RACP’s peak Indigenous health bodies, the MHC and ATSIHC, will be key facilitators for these changes.
Cultural safety is a correspondingly key attribute at the level of the organisation. Cultural safety is a concept that emerged in the late 1980s as a framework for the delivery of more effective health services for the Māori in New Zealand. Culturally safe practices include actions which recognise and respect the cultural identities of others, and safely meet their needs, expectations and rights. Conversely, culturally unsafe practices are those that “diminish, demean or disempower the cultural identity and well-being of an individual” (Nursing Council of New Zealand 2002, p. 9). There has been an increased uptake of cultural safety in medical schools in growing recognition of the value of the principles to medical practice that are contained in the framework, and their applicability to systems levels, i.e. culturally safe health services, and to the individual, whānau/family and community members Historically, health services have not been seen as safe places for indigenous people as a result of racism, cultural insensitivity, poor communication, disempowerment and historical practices, such as the removal of children.
An important principle of cultural safety is that it doesn’t ask people to focus on the cultural dimensions of any culture other than their own. Instead, cultural safety is primarily about examining the health professional’s own cultural identities and attitudes, and being open-minded and flexible in attitudes towards people from cultures other than their own.
Both cultural competence and cultural safety needs to be incorporated across all aspects of physician education, training, professional development, and practice. Training will require participants to examine their own implicit biases and to be mindful of power differentials, and have the opportunity to develop reflective practice, undertake ‘transformative’ unlearning, and contribute to a decolonisation of health services for Indigenous peoples. The RACP is in a position to develop and adopt its own Indigenous cultural competence/ cultural safety framework based on the incorporation of the principles from both concepts which most clearly reflect the of the RACP and its Indigenous health committees.
A framework for understanding Indigenous culture, health and cultural competence (originally developed by Dr Tamara Mackean, FAFPHM)
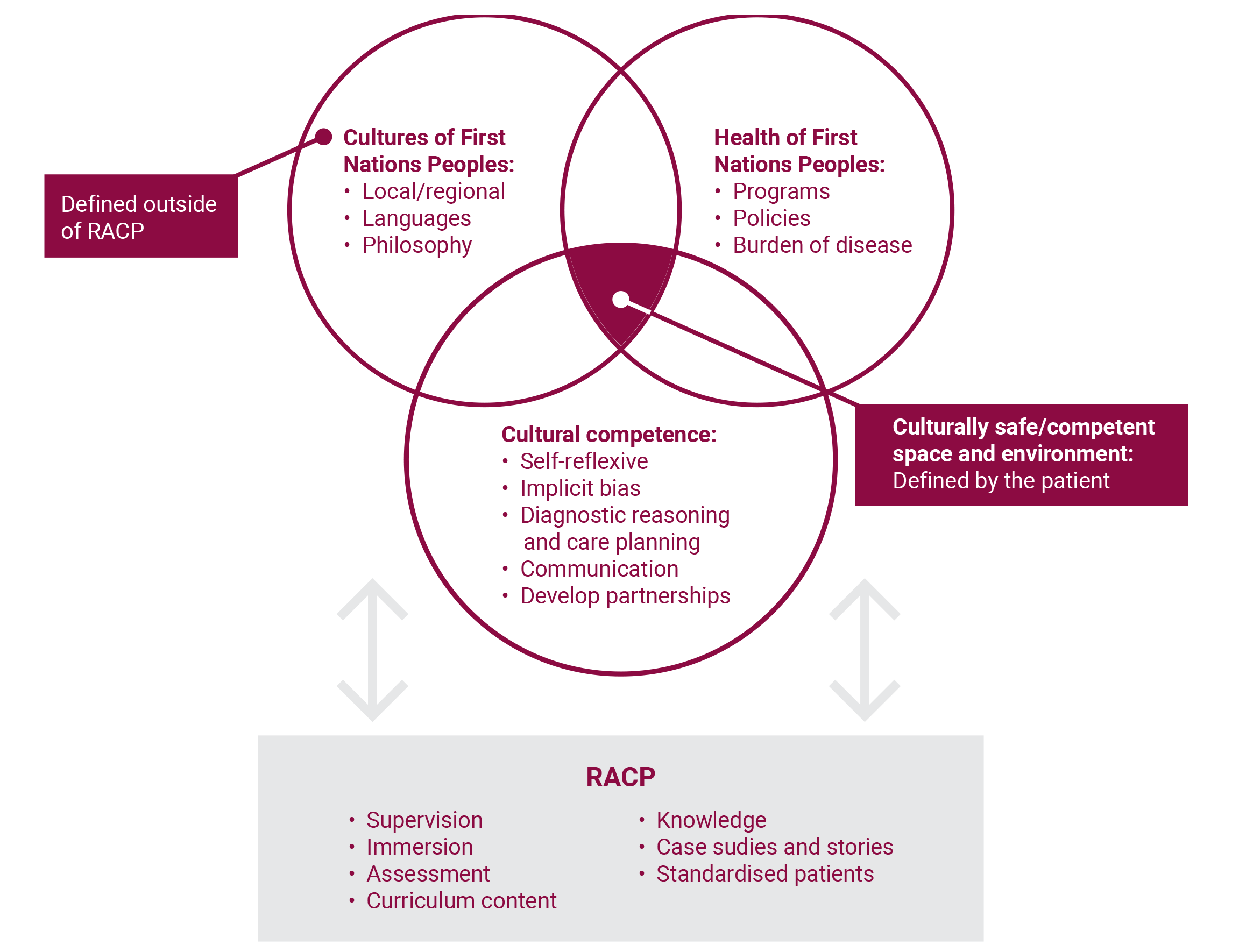
The diagram examines the generation of a culturally safe space for Indigenous Peoples, their families and their broader communities. It highlights the importance of acknowledging Indigenous world views and history, and ways the
College can foster the generation of safe environments in healthcare settings throughout Australia and New Zealand.
Strategies