The President's Message – 16 April 2021
This is a serious topic; the current outcry about the treatment of women in Australian and Aotearoa New Zealand politics, and in public life has made international news over the past month. It’s resulted in a cascade of conversations and reflections highlighting past and current misogynist and sexist behaviour. I want to make it clear that this sort of conduct is totally unacceptable in the workplace, in fact anywhere.
As physicians and trainees, we work in a wide variety of settings. We all should be aware of our own workplace codes of conduct and if applicable, public service policies. Remember, our regulators, the Medical Boards, the Medical Council of New Zealand and AHPRA have all taken a zero-tolerance approach to bullying and harassment. Our College also has a guide to behaviour in the workplace, Supporting Physicians Professionalism and Performance, which will soon be updated for your benefit.
Trainees who have concerns about harassment or bullying should raise any specific issues with either their Training Committee or the College Training Committee, the Trainees' Committee in particular, and their Director of Physician Training (DPT) if necessary.
More broadly, we have already started to look closely at the issue of gender equity within our profession. The College has established a Gender Equity in Medicine Working Group (GEM). It is working to define what gender equity means for our College members and to understand the gender equity issues for all of us.
It is examining what policies, strategies and cultures need to be addressed within our College to support gender equity overall. The GEM working group will make recommendations for change to the Fellowship Committee and the Board, and that will affect the way we all practice.
I want you to join me in making gender equity not just an aspiration, but a reality within this College.
Finally, there’s just over a fortnight to go until RACP Congress. Our Congress Program Committee has developed a COVID-safe program and delivery format. If you’re thinking twice about registering for face-to-face events because you’re concerned about possible lockdowns – don’t worry.
Come along, be part of Congress and make it a great success as it was last year.
Professor John Wilson AM
RACP President
Mā mua ka kite a muri, mā muri ka ora a mua
Those who lead give sight to those who follow, those who follow give life to those who lead
The successful applicant will join the Aotearoa New Zealand Committee. The Aotearoa New Zealand President-elect will transition to Aotearoa New Zealand President, with a position on the Board, from May 2022 to May 2024. Expressions of interest close on 4 May 2021.
For more about the position and Committee, see:
To apply, submit an expression of interest form (DOC) and CV to AotearoaNZPresident@racp.org.nz
Thank you to everyone who participated in the 2020 consultation on the proposed common learning, teaching and assessment (LTA) programs for Advanced Training (AT). Your feedback was used to refine the programs and ensure they are robust and appropriate. The common LTA programs for Advanced Training have now been finalised.
The common LTA programs will establish a baseline for learning, teaching and assessment across all AT programs. As each specialty undertakes their program-specific curricula reviews, they will build on the common LTA programs to meet the needs of their specialty.
This year, in collaboration with Curriculum Advisory Group, we will continue to support the first six specialty groups to undertake the development process:
- Cardiology (Adult Medicine)
- Cardiology (Paediatrics & Child Health)
- Gastroenterology
- Geriatric Medicine
- Nephrology
- General Rehabilitation Medicine.
Find out more

RACP Congress 2021 is just two weeks away and each city is putting its best foot forward for the occasion with an action-packed program. For those attending one of the face-to-face events, join the breakfast masterclass brought to you by William Buck and Novartis.
The daily program explores the topic of Transformation: Adapting for the future with panel discussions, orations, and clinical updates. Remember, your in-person ticket also gives you access to all the live streaming sessions, so tune in each day to stay up-to-date with the latest news.
For many of us, it has been a very long time since we have had the chance to come together and to ensure the safety and enjoyment of all attendees, all venues will follow government guidelines. We especially wish to thank our official RACP Congress technology partner Microsoft, for their support in bringing you this event.
For those wishing to attend the face-to-face event in your city, below are the final registration dates.
- Brisbane – Monday, 26 April
- Adelaide – Tuesday, 27 April
- Perth – Wednesday, 28 April
- Melbourne – Thursday, 29 April
- Sydney – Friday, 30 April
- Wellington – Wednesday, 12 May
Unable to attend in person? Register for a virtual ticket
No matter where you are, you can enjoy all that RACP Congress 2021 has to offer. Purchase a virtual ticket and live stream the entire event. Unable to attend a session? Your RACP Congress 2021 ticket includes six months of exclusive access to all recorded sessions so you can simply login and watch any missed sessions at your leisure.
Earn your CPD credits
CPD requirements have now resumed for 2021 and sessions at RACP Congress 2021 will help you achieve CPD credits in accordance with the MyCPD Framework.
The RACP virtual program includes sessions focused on professional practice such as:
- MyCPD: Practical ways to review performance and measure outcomes
- Decoding CPD: A real-life perspective on reviewing performance and measuring outcome activities
- MyCPD: Using practice data to target education and learning.
Register now

Professor Helena Teede is a clinician, academic and leader. She's an endocrinologist and n National Health and Medical Research Council fellow with a focus on women's health.
She's strongly committed to evidence based and data-driven health reform and service innovation. Professor Teede is the Executive Director Monash Partners Academic Health Research Translation Centre, Director Monash Centre for Health Research and Implementation, School Public Health, Monash University and Co-Director of Monash Institute for Health Technology which focuses on MedTech and digital health innovation.
How has digital health transformed your work?
I actively use digital health in my day-to-day work. I apply artificial intelligence and machine learning to large clinical data sets and co-develop patient interventions online and via mobile apps for lifestyle intervention programs, now running across Europe and Australia. I regularly use it to research translation mobile apps including ASKPCOS, which is now used in 112 countries and I have also used it to develop a learning health system framework using digital health technology to take practise to data, data to knowledge and knowledge to practise.
What benefits does digital health have for you on a day-to-day basis, and the industry as a whole?
Digital health technology revolutionises the way we practise healthcare identifying variation in care, gaps in evidence-based practice, identifying high-risk target populations for better care, providing a platform for low-cost evidence based interventions including supporting care in the community, coordinated specialty and primary care and sophisticated wearables and remote monitoring to name a few innovations.
Can you please share a recent example of how digital health has helped you improve patient outcomes?
We have co-designed a translation resource linked to our leadership of an international guidelines for polycystic ovary syndrome developed across 71 countries and are used across 146 countries. The translation resource ASKPCOS is now used internationally with extensive uptake and reach, to improve patient knowledge and help optimise patient provider interactions to optimise health outcomes.
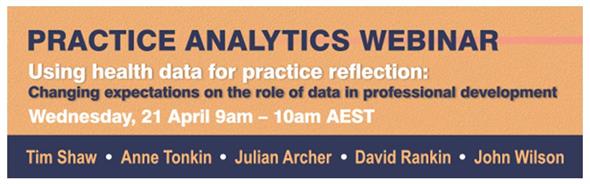
The Digital Health Cooperative Research Centre is kicking off a series of virtual events covering hot topics in the field of practice analytics. The first webinar will be held on Wednesday, 21 April 2021 from 9am (AEST) and will explore the potential use of health data for practice reflection and professional development. The event will consider how this aligns with the Medical Board of Australia’s Professional Performance Framework.
The panel will include Professor John Wilson AM (RACP President), Anne Tonkin (Medical Board of Australia Chair), Adjunct Professor Julian Archer (Executive General Manager for Education, Royal Australasian College of Surgeons), Dr David Rankin (Director Clinical Governance and Informatics, Cabrini Health) and chaired by Tim Shaw (Director of Research, Digital Health CRC).
Register now
By now, you may be familiar with your specialties’ Evolve ‘Top-5’ recommendations and now want to share them with your students, early-career clinicians and even colleagues and Fellows. How will you engage others to drive high-value, high-quality care?
Join Dr Chris Leung on Tuesday, 27 April 2021 from 6pm to 7pm (AEST), or from 8pm to 9pm (NZST), as he shares the innovative strategies he uses to engage his team, from hospital inductions to gamification. Dr Leung has trialed multiple approaches to ensure patients are receiving the tests, treatments and procedures they need and not those they don’t.
Register now
Fellows and trainees of all specialities are invited to enrol in this new Qstream course, which has a mid-May start. The course is designed to provide practical strategies to help you enhance your teaching skills and effectively balance teaching with a busy workload.
You'll access in-depth case studies with questions that are sent directly to your inbox at spaced intervals over a three-week period. Each question takes just ten minutes to complete, and participants are encouraged to discuss the case studies and share opinions with others through secure, online discussion forums.
The course is designed to enhance your knowledge in adult learning, provide practical strategies to incorporate effective teaching skills into day-to-day settings, and encourage self-reflection and peer discussion.
Enrol now
Physicians often fail to put on their own oxygen masks when dealing with the challenges and stresses that come with practising during a pandemic. This online course explores in-depth how to better support your own wellbeing, as well as the wellbeing of your staff and colleagues through compassionate leadership. The course covers concepts, strategies, and tools to help you mitigate the impact, set healthy boundaries, prevent burnout, and build support networks during a crisis.
Enrol now
A recent audit of multidisciplinary paediatric weight management services in Australia has shown that their current availability and accessibility are inadequate to service children and adolescents with obesity. In particular, those with severe obesity and those in rural and remote communities.
Despite a small increase in the number of multidisciplinary paediatric weight management services since the last audit in 2008, current services have waitlists of up to 12 months and no multidisciplinary services are available in rural or remote communities.
Audit results demonstrate the urgent need for additional multidisciplinary services, improved training for healthcare professionals and better monitoring of the provision of evidence-based care to better address the issue of paediatric obesity in Australia.
Learn more
RACP members and stakeholders who have published in the field of Indigenous health research within the last five years are invited to participate in a survey being conducted by the University of Melbourne School of Population and Global Health.
The purpose of the research is to understand Australian researchers’ perspectives regarding use and application of ethical guidelines with attention to governance as a foundation for ethical Indigenous health research.
What is involved?
This multi-choice survey takes 10 to 15 minutes to complete and closes on Sunday, 9 May 2021. It has received Ethics approval from the University of Melbourne School of Population and Global Health Human Research Ethics Committee and all data collected will be deidentified. Your involvement in the survey will contribute to a vital area of research that aims to improve the application of ethical guidelines to research involving Aboriginal and Torres Strait Islander people.
Please contact Lead Investigator Associate Professor Luke Burchill (Yorta Yorta / Dja Dja Wurrung) for further information.
Encouraging conversations around end-of-life can be challenging, but a new video, Discussing choices: Indigenous advance care plans: A Learning resource shows that conducting culturally-safe end-of-life discussions is a skill that can be learnt.
Palliative Care Australia with the collaboration from the Groote Eylandt community recently launched the video which offers learnings and tips for health professionals on how to conduct culturally-sensitive discussions on advance care planning and end-of-life care with Aboriginal and Torres Strait Islander people.
Warning: Aboriginal and Torres Strait Islander people may find content in this film upsetting.
Watch the video
Join the online launch of the Fourth Australian Atlas of Healthcare Variation on Wednesday, 28 April from 12pm to 1pm (AEST).
National healthcare leaders including Professor John Newnham AM, 2020 Senior Australian of the Year and Professor in Obstetrics and Gynaecology at The University of Western Australia, will share key findings from the new Atlas and explain what they reveal about the appropriateness and equity of healthcare delivery in Australia.
Produced in partnership with the Australian Institute of Health and Welfare, the Atlas identifies variation for a range of procedures, investigations, treatments and hospitalisations. With recommendations to reduce unwarranted variation, it provides opportunities to minimise low value care, improve the equity of care and improve patient outcomes.
Register now

We’re hosting more online events than ever before, so have introduced a condensed monthly events digest. The first one was sent to you on 7 April, but you can also read it online.
This monthly communication will be sent to you on the first Wednesday of each month, to provide you with an opportunity to virtually attend events from all over Australia and Aotearoa New Zealand. We hope this makes your life a little easier and we look forward to seeing you at our next event.
Read the April events digest
 This is the third and final part of the series on gendered medicine. We step back and look at the way that health care and research are funded. It’s been said that the health needs of women are undervalued by our existing fee-for-service model, down to individual item numbers in the Medicare Benefits Schedule. There’s also evidence that disease predominantly experienced by female patients receive less research investment. Is this blatant sexism or a symptom of structural imbalance, and what do we do about it?
This is the third and final part of the series on gendered medicine. We step back and look at the way that health care and research are funded. It’s been said that the health needs of women are undervalued by our existing fee-for-service model, down to individual item numbers in the Medicare Benefits Schedule. There’s also evidence that disease predominantly experienced by female patients receive less research investment. Is this blatant sexism or a symptom of structural imbalance, and what do we do about it?
Guest
Dr Zoe Wainer BMBS, PhD, MPH (Director of Clinical Governance, BUPA)
Listen now
The April 2021 Journal of Paediatrics and Child Health is now available. One of the highlights is a viewpoint article, Embedding clinical trials within routine healthcare delivery: Challenges and opportunities.
Other key highlights include:
- The precautionary principle, the AstraZeneca COVID‐19 vaccine and mixed messaging
- Paediatric genomic testing: Navigating Medicare rebatable genomic testing
- Proopiomelanocortin deficiency diagnosed in infancy in two boys and a review of the known cases
- Play and medical play in teaching pre‐school children to cope with medical procedures involving needles: A systematic review
- Diagnosis and management of paediatric Clostridioides difficile infection in a tertiary centre: A prospective audit
- Factors related to passing the safety fast test among neonates with hypoglycaemia in the neonatal intensive care unit
- Relationship between patient understanding and timeliness of penicillin prophylaxis in rheumatic heart disease prevention programmes in American Samoa
- Revealing the clinical phenotype of atypical neuronal ceroid lipofuscinosis type 2 disease: Insights from the largest cohort in the world.
Read now
 The need for healthcare providers to connect to each other safely and securely is greater than ever. Secure messaging is an efficient and timely method for sending and receiving clinical information, which minimises the burden of paper and manual processes. An increased uptake of secure messaging improves continuity of care for patients, saves time and can help protect vital health information.
The need for healthcare providers to connect to each other safely and securely is greater than ever. Secure messaging is an efficient and timely method for sending and receiving clinical information, which minimises the burden of paper and manual processes. An increased uptake of secure messaging improves continuity of care for patients, saves time and can help protect vital health information.
Safety and Quality Benefits of Secure Messaging
The content in this document has been derived from a review undertaken by the clinical safety program conducted by the Australian Commission on Safety and Quality in Health Care, on behalf of the Australian Digital Health Agency.
Download now (PDF)
Expressions of Interest are still open for Fellows in the Adult Medicine and Paediatric & Child Health Divisions to join our team of accreditors. As an accreditor, you play a vital role in ensuring the delivery of high-quality workplace training. Your contribution to accreditation can also count towards your annual CPD credits.
Please submit an Expression of Interest (EOI) form by Wednesday, 30 June to accreditation@racp.edu.au (Australia) or accreditation@racp.org.nz (Aotearoa New Zealand).
Stay informed
Read other RACP eBulletins: